
The biggest mistake I see students make with rotations is this: they treat them as auditions for a specialty, not as test-drives for the type of residency and career they are signing up for. Community vs academic fit will affect your daily life far more than whether you match at Hospital A or B.
You are not just choosing a program. You are choosing a system, a culture, and a pace of life. Rotations are your only real chance to try both on before the Match locks you in for years.
This is the playbook for doing that properly.
Step 1: Get Clear On What “Community vs Academic” Really Means
Forget the brochure language. Strip it down to what you will actually feel on a Tuesday at 3 p.m.

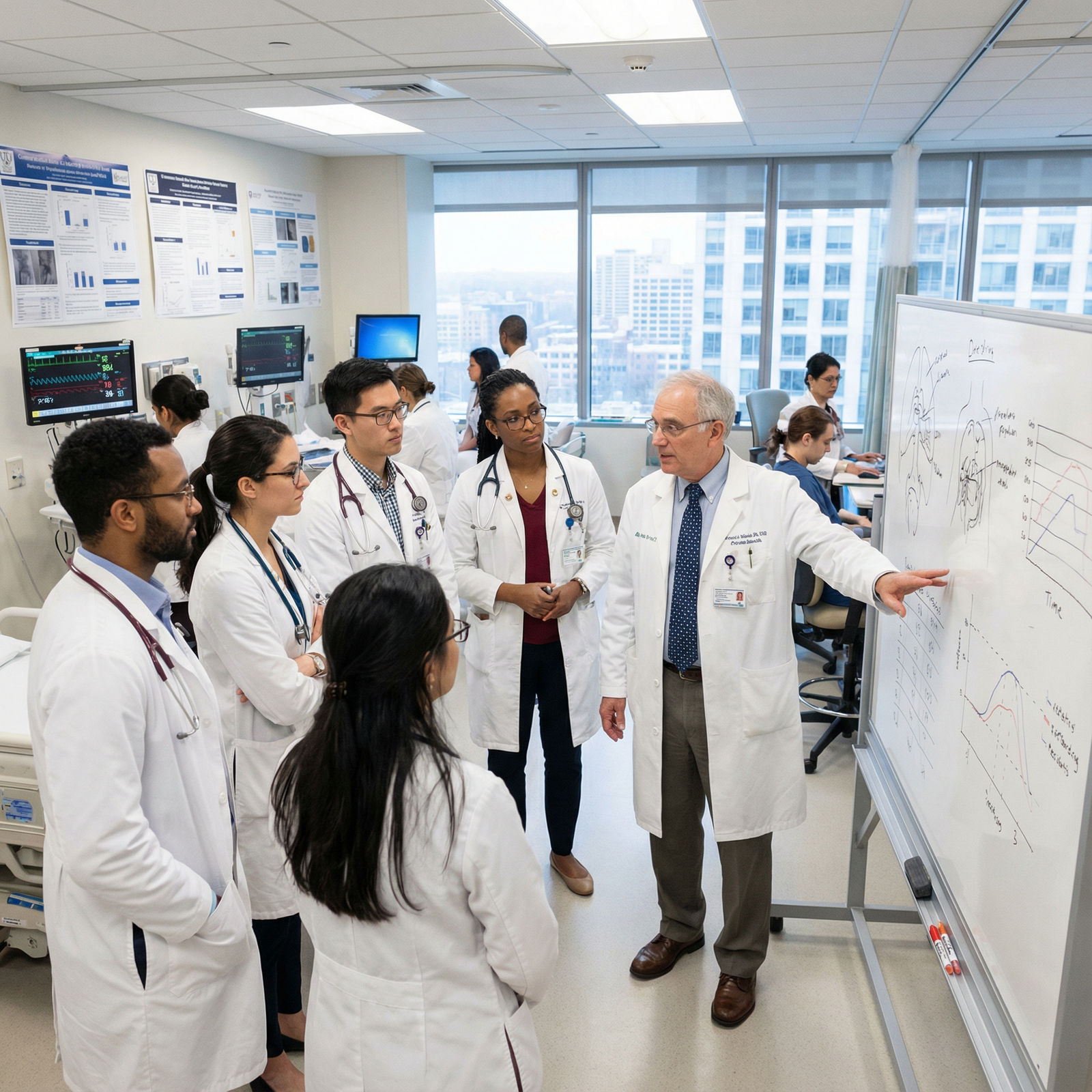
What Academic Programs Usually Feel Like
Academic centers tend to have:
- Big quaternary referral hospitals
- Subspecialists everywhere
- Research expectations (or at least pressure)
- Layers of learners (students, residents, fellows)
- Strong emphasis on guidelines, conferences, and evidence-heavy discussions
Typical daily experience:
- Longer formal teaching: noon conference, morning reports, journal clubs.
- More consults and complex, rare pathology.
- More bureaucracy: committees, protocols, EMR rules.
- More people in the room: students, fellows, advanced practice providers, residents from other services.
Upside: constant learning, prestige, subspecialty doors wide open.
Downside: you can feel like a cog in a huge machine. Less autonomy early.
What Community Programs Usually Feel Like
“Community” is a spectrum. Some are very academic-lite; others are true private-hospital workhorses.
Common features:
- Smaller or mid-sized hospitals
- Fewer or no fellows
- Attendings more likely in private practice groups
- Less research infrastructure
- Patients mostly from the surrounding region, less zebras, more bread-and-butter
Typical daily experience:
- You are needed for throughput. Your notes, orders, and discharges are integral to flow.
- Attendings know you by first name and may call your cell.
- Teaching can be excellent, but less formal and structured.
- You may be the only resident on a service or at night.
Upside: autonomy, volume of common problems, early responsibility, closer relationships.
Downside: fewer niche subspecialty mentors, less protected time, less “academic currency” if you want big-name fellowships.
Why You Must Decide What You Actually Want
Before you start “testing” with rotations, you need working hypotheses:
- Do you see yourself:
- Running trials / publishing regularly? → Lean academic.
- Being the community workhorse everyone calls? → Lean community.
- Unsure → You must sample both worlds intentionally.
Write this out. Literally. One page, two columns: “I want” vs “I do not want.”
That sheet is your anchor for the rest of this playbook.
Step 2: Design Your Rotation Strategy (Not Just What Will Impress ERAS)
Here is where most students blow it: they let the school scheduler or random availability decide what exposures they get. Then six months later they say, “I guess I liked both?” That is useless.
You need a deliberate mix.
| Phase | Rotation Type | Setting |
|---|---|---|
| Core (MS3) | Internal Medicine | Academic |
| Core (MS3) | Surgery or OB/GYN | Community |
| Elective (MS4) | Sub-I in target specialty | Academic |
| Elective (MS4) | Sub-I or AI in same specialty | Community |
| Elective (MS4) | Research or niche elective | Academic |
If you are already in late MS3 or MS4, you work with what you have, but aim for at least one solid month in each environment in your intended specialty or something close to it.
Priorities When Picking Rotations
At least one academic rotation in your specialty or closely related field.
You want to see pure academic culture. Think: university hospital, busy teaching service, real attendings who publish.At least one community rotation with residents (not just private practice shadowing).
You are testing residency style, not just attending lifestyle. You need to see:- How residents are used
- How teaching is or is not built in
- How the schedule feels
Ideally, a Sub-I / Acting Internship in both settings.
On a Sub-I, you feel closer to resident reality: cross-cover, admissions, running a list. That matters for fit.
If you cannot get perfect symmetry, fine. But aim for it and push hard with your dean’s office to approximate it.
Step 3: Use a Structured Observation Checklist (Not Vibes)
Rotations are chaotic. You are tired. You latch onto random impressions: “The food was good,” “The residents seemed nice,” “The call room sucked.”
That is how you end up matching into the wrong environment.
You need a checklist. Use this every single day and capture quick notes on your phone or small notebook. Do not rely on memory.

| Category | Value |
|---|---|
| Resident autonomy | 8 |
| Teaching quality | 7 |
| Workload intensity | 9 |
| Research visibility | 9 |
| Fellow presence | 10 |
| Clinic vs inpatient balance | 6 |
Core Domains to Track
Autonomy vs Oversight
- Who actually writes orders?
- Who talks to consultants first—resident or attending?
- Are residents allowed to make plans and then review, or do attendings dictate everything?
Teaching Culture
- Is teaching scheduled and protected, or just “on the fly” when there is time?
- Do attendings ask you questions just to pimp, or to teach?
- Are residents teaching each other, or just surviving?
Workload and Support
- Average census per resident.
- Presence of APPs or hospitalists lightening the load.
- Time to sit and think vs constant fires.
Breadth and Depth of Pathology
- Are you seeing rare diseases almost weekly (academic pattern)?
- Is it mostly common conditions with high volume (community pattern)?
- Do you feel intellectually stretched, or mechanically busy?
Research and Academic Activity
- Do residents talk about projects in the workroom?
- Are conferences referencing local data, QI work, or trials from your own institution?
- Does anyone ask about your research interests?
Program Culture
- Do residents eat together or disappear as soon as the work is done?
- How do they talk about leadership when leadership is not around?
- Are you hearing “burnout” jokes every day?
System Red Flags
- Chronic understaffing: residents covering 3 people’s work.
- Open hostility between services.
- Constant admission of “We do not have time to teach here.”
Make these domains into a simple 1–5 rating you fill out weekly. You are building data, not just impressions.
Step 4: Learn To Read Residents And Attendings Correctly
You are not just observing institutions. You are reading people. Because your future will look like them.
How To Read Residents
I listen for specific lines:
Academic setting red flags:
- “I have no time to do my research; I will deal with it as a fellow.”
- “I am just here to get a fellowship and leave.”
- “We are basically scut monkeys for the fellows.”
Academic setting positives:
- “Our chair helps us get data quickly.”
- “Everyone matches into strong fellowships from here.”
- “Our program director really shields our academic time.”
Community setting red flags:
- “Teaching is whatever is left after throughput.”
- “We are basically covering what three hospitalists used to do.”
- “We are always short-staffed at night.”
Community setting positives:
- “I feel very ready for independent practice.”
- “Attendings let me run the list and make decisions.”
- “The program leadership actually knows all of our personal situations.”
Pay attention not just to what they say, but when they say it:
- End of a 28-hour call rant is different from a calm conversation at noon conference.
How To Read Attendings
Academic attendings:
- Do they discuss guidelines and primary literature at the bedside?
- Or do they seem disengaged and let fellows do all the teaching?
- Are they involved in resident feedback and career planning, or just in their own research bubble?
Community attendings:
- Are they willing to slow down and talk through “why” behind decisions?
- Or are they clearly on RVU autopilot with minimal teaching?
- Do they view residents as future colleagues or as cheap labor?
Strong sign you fit an environment: you find yourself thinking, “I would not hate becoming like this person in 10–15 years.”
If you cannot find anyone like that in a given setting, pay attention.
Step 5: Run A Daily / Weekly Debrief System
Reflection without structure dissolves into vague feelings. You need a simple, repeatable process.
Daily 5-Minute Debrief
At the end of each day, answer these 5 prompts:
- What felt energizing today?
- What drained me the most?
- When did I feel like a real doctor-in-training?
- When did I feel invisible or unnecessary?
- Academic vs community style—did today push me more toward one?
Do not write paragraphs. Write bullet fragments. Keep a running note on your phone.
Weekly Fit Score
Every weekend on a rotation, score the rotation on:
- Workload sustainability (1–10)
- Educational quality (1–10)
- Culture/people fit (1–10)
- Future-you alignment (1–10): “Can I see myself here or in a place like this for 3–7 years?”
Then, assign:
- A for “I would be happy here”
- B for “Acceptable, not ideal”
- C for “Hard no”
Pattern you are looking for:
- If all your academic rotations rate A/B and community are C → you are probably an academic fit.
- Reverse → you are likely a community fit.
- Mixed → you need to interrogate why certain ones clicked and others did not.

| Category | Academic IM | Community IM | Academic Surgery | Community FM |
|---|---|---|---|---|
| Week 1 | 7 | 5 | 4 | 8 |
| Week 2 | 8 | 6 | 5 | 8 |
| Week 3 | 8 | 6 | 5 | 9 |
| Week 4 | 9 | 5 | 4 | 9 |
When you see the graph in your own data, the pattern usually stops being ambiguous.
Step 6: Use Rotations To Test “Real Life” Issues, Not Just Medicine
Lifestyle is not shallow. It is survivability.
Schedule And Workload Reality Checks
On each rotation, explicitly track for one full week:
- Average daily work hours (door-to-door)
- Commute time
- Number of days with:
12 hours in hospital
- Skipped meals
- Charting at home
Compare across your academic and community rotations. Do not be shocked when community + no fellows = more raw service work. Sometimes that is fine. Sometimes it is a breaking point.
Geography And Community Feel
Community programs are often in smaller cities or suburbs. Academic in bigger metros.
Notice:
- Do you like the pace, cost of living, and traffic near the community site?
- Or do you feel restless and trapped?
- Conversely, does the big academic center feel energizing or exhausting?
Use your off days. Walk around nearby neighborhoods. Eat somewhere outside the hospital cafeteria. Ask residents where they actually live.
You are testing a life, not just a program.
Step 7: Align Your Rotation Story With Your Application Strategy
You are not just doing rotations to decide how you feel. You are creating a coherent story you can tell in your personal statement, ERAS, and interviews.
If You Are Leaning Academic
You want rotations that demonstrate:
- Comfort and success in academic centers:
- Strong evaluations from academic attendings.
- Participation in research, QI, or teaching.
- Understanding of what academic life actually looks like:
- You can reference real experiences with M&M, journal clubs, QI projects.
Translate your test-drive into language like:
- “Across rotations in both community and academic settings, I found I thrived in environments with robust subspecialty exposure and regular case-based conferences.”
- “Working on my Sub-I at [Academic Hospital], I saw how integrated research and clinical care can accelerate answers for complex patients.”
If You Are Leaning Community
You want:
- Rotations that show:
- High-volume, bread-and-butter experience.
- Clear examples of autonomy and early responsibility.
- Concrete proof you value patient access, continuity, and efficiency.
Translate into statements like:
- “At [Community Hospital], I experienced the satisfaction of managing common conditions at scale and becoming a reliable point person for the team.”
- “I realized I want a program where resident autonomy grows rapidly, and I felt that most strongly in my community Sub-I rotation.”
If You Want To Keep Both Options Open
Fine. But do it intentionally.
- Apply to a mix of community and academic programs.
- Prepare two slightly different angles for interviews:
- Academic programs: emphasize teaching, research, and complex care.
- Community programs: emphasize autonomy, efficiency, and team integration.
What you do not do: give every interviewer the same vague “I just want good training” line. They have heard that 10,000 times.
Step 8: Identify Absolute Dealbreakers Early
You will not find a perfect program. But there should be hard lines you are not willing to cross.
Rotations are where you test these. Some examples:
Academic Dealbreakers
- Residents openly say, “The fellows do all the good cases, we just admit and discharge.”
- Zero support for research despite heavy lip service.
- Chronic violation of duty hours.
- Toxic hierarchy where students and interns are publicly humiliated daily.
Community Dealbreakers
- No consistent didactics, everything “optional” and barely attended.
- You never see an attending teach, only bark orders.
- Residents doing nonstop service with no time to think or study.
- Program leadership invisible or indifferent to resident concerns.
When you spot a dealbreaker in a rotation, write it down with context. Later, when comparing programs, remember: anything you see on a 4-week rotation is often milder than what residents live with for 3–7 years.
Step 9: Talk To The Right People, The Right Way
You will not fully understand a program just from your own vantage point. You need to ask strategic questions without sounding like you are interrogating anyone.

| Step | Description |
|---|---|
| Step 1 | Start Rotation |
| Step 2 | Week 1 - Observe quietly |
| Step 3 | Week 2 - Ask residents casual questions |
| Step 4 | Week 3 - Deeper questions with trusted seniors |
| Step 5 | Week 4 - Ask attendings about long term paths |
Questions For Residents (Off the Record)
Skip the generic “Do you like it here?” Ask:
- “If you could remake this program from scratch, what would you keep and what would you ditch?”
- “Where do graduates end up? Jobs? Fellowships? Are they generally happy?”
- “On a scale of 1–10, how much would you push your best friend to come here?”
- “What type of student thrives here and what type struggles?”
And specifically for community vs academic testing:
- Academic residents:
- “How much of your time feels like genuine learning vs service?”
- “Do you feel prepared for community practice too, or mainly academics?”
- Community residents:
- “If you wanted a competitive fellowship, how supported do you feel?”
- “How early did you start feeling like you could run things independently?”
Questions For Attendings
You are not asking them to trash their own program. You are eliciting how they see it.
- “What kind of resident does best in this environment?”
- “How would you describe this program’s place on the community–academic spectrum?”
- “If a resident here wants to go into academics / private practice, how do you support that?”
Their answers tell you:
- Whether they are self-aware.
- Whether they are honest about limitations.
- Whether your own path aligns with what the program actually does well.
Step 10: Synthesize Everything Into A Clear Direction Before You Submit ERAS
Here is where you fix the core problem: going into ERAS without a strong sense of environment fit.
By the time applications open, you should be able to answer:
Do I want:
- Primarily academic programs?
- Primarily community programs?
- Or a deliberate mix of both?
If a program is “hybrid” (community-based with academic affiliation), what side should it lean toward for me to be happy?
What 3–5 non-negotiable features must my programs have?
- Example: “No fellows in my core specialty” or “Strong research infrastructure with protected time.”
Take your rotation notes, weekly scores, and conversations. Sit down for one dedicated evening and force yourself to create:
- A ranked list of:
- Pure academic environments
- Pure community environments
- Middle-ground / hybrid programs
Pre-ERAS, you are not picking program names yet; you are picking buckets you will target.

Three Takeaways To Keep
Use rotations as structured experiments, not just as hoops to jump through. Track autonomy, teaching, workload, culture, and your own energy systematically across community and academic settings.
Read the people as much as the place. Residents and attendings are living previews of your future. If you do not want their life, do not choose their environment.
Decide on your environment before you submit ERAS. Design your rotation mix, reflection process, and conversations so that by application time, you know whether you are aiming for community, academic, or a very specific mix—and why.




















