
The third-year surgical clerkship will quietly decide whether you match ortho, ENT, or plastics—months before you ever open ERAS.
If you treat MS3 like “I’m just figuring it out,” you will lose ground to classmates who are already acting like future applicants. These fields reward people who treat time like a weapon. You need to know exactly which weeks matter, what has to be locked in, and when a decision stops being “early exploration” and becomes “you’re now behind.”
I am going to walk you from the first day of MS3 through the end of the year, with explicit checkpoints where your decisions for ortho, ENT, and plastics either stay alive—or quietly die.
Big Picture: The Competitive Clock You Are On
Before the week‑by‑week, understand the pressure you are under.
For ortho, ENT, and plastics, your “real” application is not ERAS. Your real application is:
- Clerkship evals from surgery and subspecialty rotations
- Who will write your letters (and how well they actually know you)
- How early you commit to away rotations and home sub‑internships
- Whether you decide your specialty early enough to build a coherent story
The brutal part: most of this is decided between Month 1 and Month 9 of MS3. Long before ERAS submissions.
Here is how the competitiveness shakes out.
| Specialty | Approx. Applicants:Positions | Step 2 CK Target Range | Away Rotations Typical |
|---|---|---|---|
| Ortho | ~1.3–1.5:1 | 245–255+ | 2–3 |
| ENT | ~1.4–1.6:1 | 245–255+ | 2–3 |
| Plastics (Integrated) | 1.7–2.0:1 | 250–260+ | 2–3 |
You cannot control the ratio. You can control when you start moving like a serious applicant.
MS3 Month 1–2: Set the Board Before the First Cut
At this point you should stop thinking “surgical” in general and start testing specific directions.
Weeks 1–2 of MS3: Reality Check and Early Positioning
Whether you start on internal medicine, surgery, or something else, your first two weeks set the tone.
You should:
Get honest numbers and risk profile.
- Confirm Step 1 result (if P/F, fine, but know where you stand in your class).
- Estimate Step 2 CK goal range based on your test history.
- Ask your academic advisor one direct question:
“If I want ortho/ENT/plastics, what would make you nervous about my application right now?”
Clarify which of the three is even plausible.
- If you have no prior interest and no surgical exposure, choosing integrated plastics out of nowhere in Month 10 of MS3 is fantasy.
- If you already shadowed ortho or ENT in pre‑clinical years, lean into that early.
Line up a mentor in each serious option.
- One ortho faculty (or senior resident).
- One ENT faculty.
- One plastics faculty.
Email them now. Short and direct. Ask for a 20–30 minute conversation about planning an application, not “can you get me in.”
At the end of Week 2, you should have a short list:
- Primary interest: e.g., Ortho
- Secondary “possible pivot”: ENT or general surgery
- Tertiary “safety” idea (if your metrics are marginal): IM, anesthesia, etc.
You are not marrying anyone yet. But you are not “I like surgery broadly” anymore. That vague phase is over.
MS3 Surgery Block: The Rotation That Makes or Breaks You
If you want ortho, ENT, or plastics, your core surgery clerkship is not just another rotation. It is your first audition.
Pre‑Surgery Block (2–4 Weeks Out)
At this point you should:
- Identify your surgery block dates and any built‑in subspecialty weeks (ortho, ENT, plastics, vascular, etc.).
- Tell your mentors when your surgery block starts and ask:
“Which teams should I request if I am interested in [specialty]?” - Fix your life logistics – surgery hours will fight your study time and Step 2 prep if you do not plan ahead.
Week 1 of Surgery: First Impressions
Your only job this week:
- Show that you are the student attendings want back as a sub‑I.
- Ask the chief and senior residents:
“I am really interested in [ortho/ENT/plastics]. What can I be doing this month to be the best possible student and position myself for sub‑Is?”
What you must not do:
Wait silently for people to “discover” your interest. They will not. Everyone is too busy.
Weeks 2–4 of Surgery: Subspecialty Windows
Most schools give you 1–3 weeks of subspecialty exposure. These weeks are critical for triage:
- On ortho week:
- Ask the residents about the ortho match from your school.
- Pay attention to what they say about research expectation and away rotations.
- On ENT or plastics week (if you get one):
- Show up early to every OR. ENT and plastics notice punctuality and prep.
- Ask 1–2 smart, concise questions per day. No more. No rambling.
At the end of your subspecialty weeks, you should be able to answer:
- Did I like the daily life, or just the idea of the specialty?
- Did any faculty or residents seem genuinely enthusiastic about helping me?
- Does the culture fit my personality?
This is where a lot of people lie to themselves. They chase prestige instead of the actual day‑to‑day. That mistake shows up as burnout in PGY2.
Mid‑Surgery Block: Month 4–5 of MS3 – Commit to a Direction
Around the midpoint of your surgery clerkship, the clock changes. You go from exploration to early commitment.
At this point you should:
Pick a working primary specialty.
- Example: “I am going to act as if I am applying ortho, and keep ENT as a backup idea.”
This does not mean you can never switch. It means you stop drifting.
- Example: “I am going to act as if I am applying ortho, and keep ENT as a backup idea.”
Identify 2–3 letter‑of‑recommendation targets.
- An attending or two on your core surgery service.
- A subspecialty attending in your area of interest.
You are not asking for letters yet. You are collecting potential writers.
Start low‑friction research conversations.
- Ask residents: “Is there a case report or small project I can help with?”
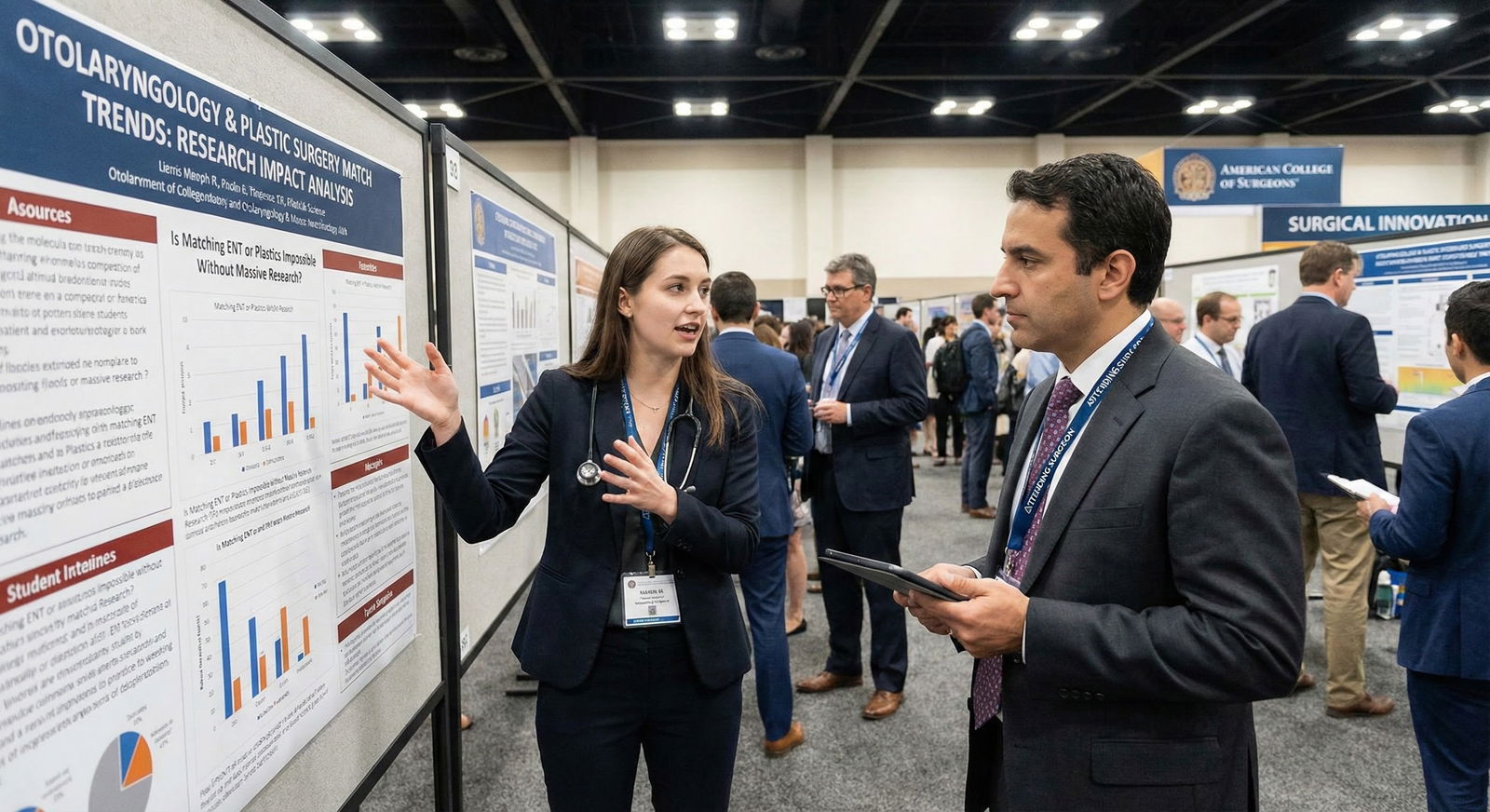
You do not need a full bench research empire. You need something — especially for plastics and ENT, where research volume is absurd.
- Ask residents: “Is there a case report or small project I can help with?”
End of Core Surgery: The First Hard Checkpoint
The last 1–2 weeks of your surgery block are a decision window.
Your Goals Before the Rotation Ends
- Secure at least one strong clinical advocate who would be happy to see you on a sub‑I.
- Have at least one subspecialty team where someone knows your name and work ethic.
- Get HONORS if it is within reach. For these fields, a Pass in core surgery is a handicap. Not fatal, but you will now need to compensate with Step 2, sub‑I performance, and research.
At this point you should schedule follow‑ups:
- 15‑minute meeting with your preferred specialty mentor to debrief:
“Given how I did on surgery, how realistic is [ortho/ENT/plastics] for me?” - Ask directly if your current trajectory is competitive.
If the answer is “You are borderline,” do not ignore it. That is your early warning to either:
- Double down on metrics (Step 2, research, away rotations), or
- Start exploring a more realistic alternative in parallel.
MS3 Months 6–7: Sub‑I Planning and Away Rotations – The Invisible Deadline
Away rotations for ortho, ENT, and plastics often open ERAS‑like: applications going in late winter/early spring of MS3, for rotations in summer/early fall of MS4. If you wait until everyone is talking about ERAS, you are already late.
At This Point You Should Lock Down:
- Home Sub‑I Plan
Figure out:
- When you will do a home sub‑I in your chosen field (or the closest available).
- Which month(s) your school allows sub‑Is.
- The ideal order: often home sub‑I first, then aways, so you do not show up clueless at other institutions.
- Away Rotation Targets
You should have:
- A short list of 4–6 programs you would be proud to match at.
- At least 2–3 realistic aways you plan to apply to in your chosen specialty.
Do not carpet‑bomb 15 aways. Programs talk. You look scattered. And you will be exhausted.
- Backup Plan Logic
If you are still torn between two of the big three:
- Example: Torn between ortho and ENT.
- Pick one as your “front‑runner” and aim aways in that specialty.
- Keep a route open to pivot to the other with a late sub‑I if absolutely necessary.
Here is what the timeline pressure often looks like.

| Category | Value |
|---|---|
| MS3 Start | 0 |
| After Surgery Clerkship | 25 |
| Mid MS3 | 60 |
| End MS3 | 85 |
| Early MS4 | 100 |
Think of that line as “percent of your final competitiveness story written.” By early MS4, it is almost done.
MS3 Months 7–9: The Fork in the Road Window
This is the stretch where people panic and start switching specialties. Some switches are smart; some kill applications.
At this point you should:
1. Re‑Evaluate Based on Real Data
Look at:
- Your core surgery grade and narrative comments.
- Any early subspecialty feedback (“One of the best students we’ve had this year” vs “quiet, did what was asked”).
- Whether any faculty spontaneously say, “Are you thinking about [specialty]? You should.”
Then be honest:
- If you have strong feedback, good grades, and a competent Step 2 practice trajectory – you can push forward confidently in ortho/ENT/plastics.
- If you are struggling on shelves, average on the wards, and have weak feedback – trying to force integrated plastics with zero research is denial.
2. Decide: Commit, Pivot Within Surgical, or Step Down in Competitiveness
Three pathways:
Commit fully to ortho/ENT/plastics.
- Lock in aways.
- Double down on research.
- Tell mentors clearly: “I am all‑in.”
Pivot within surgical – e.g., from plastics fantasy to general surgery or from ENT to anesthesiology.
- You can still use your surgery momentum.
- You will have more breathing room and fewer away requirements.
Step down to a non‑surgical or less competitive field if needed – but do it early, with intention, not after 3 failed aways and no interviews.
The dangerous move is pretending you are in group 1 when your objective data scream group 2 or 3.
Daily and Weekly Habits During MS3 That Actually Move the Needle
This is where students either quietly build a lethal application…or drift.
Weekly
At this point each week you should:
Touch your specialty in some way.
- One research task.
- One journal article.
- One focused shadowing half‑day if possible.
Document wins and feedback.
Keep a running doc of:- Patient encounters you led.
- Complex cases you followed.
- Positive quotes from attendings or residents.
This is the raw material for letters and personal statements later.
Check in with one mentor every 4–6 weeks.
Send a short update:- What rotation you are on.
- One concrete win.
- One specific question (e.g., “Does it matter if my first away is August vs September?”).
Daily (On Surgical Rotations)
You do not need a fancy system. You need consistency:
- Show up before the residents.
- Know your patients cold.
- Read one short topic most nights related to your OR cases the next day.
- Ask for feedback mid‑rotation, not just at the end.
None of this is glamorous. But this is exactly how students end up with “best student of the year” comments that rescue them from a slightly low Step 2 or an average research portfolio.
When You Are Between Two (Ortho vs ENT vs Plastics) Too Long
Staying indecisive has a cost.
Signs You Are Waiting Too Long to Choose
- It is Month 8–9 of MS3 and you still say, “I’m between ortho, ENT, and plastics, just seeing what happens.”
- You have not applied to any aways because “I might change my mind.”
- No letter writer could say, “I have worked with this student extensively in [field].”
If you recognize yourself here, you need a 7‑day decision sprint:
- Meet with mentors in each specialty.
- Ask each: “If I were your kid, would you tell me to go for this field based on my current record?”
- Decide by the end of the week.
Not a perfect decision. A workable one that allows you to build a coherent application.
Visualizing the Year: Your MS3 Surgical Decision Timeline

| Period | Event |
|---|---|
| Early MS3 - Month 1-2 | Identify mentors and serious interest areas |
| Early MS3 - Month 2-3 | Complete or begin core surgery |
| Mid MS3 - Month 3-5 | Subspecialty weeks, initial commitment |
| Mid MS3 - Month 5-6 | Finish surgery, choose working primary specialty |
| Late MS3 - Month 6-7 | Plan home sub-I and aways |
| Late MS3 - Month 7-9 | Commit or pivot, solidify letters and research |
Keep that structure in your head. Every time you drift, ask: “What part of the timeline am I on, and what should I be doing right now?”
How These Choices Hit Your Match Odds
To ground this, think in terms of match probability rather than vague “competitiveness.”

| Category | Value |
|---|---|
| Late Decider, Minimal Research | 35 |
| Mid-Year Decider, Some Research | 55 |
| Early Decider, Strong Mentorship | 75 |
These are not official NRMP statistics. They reflect what I have seen repeatedly:
- Students who decide early, build relationships, and perform on surgery crush it.
- Students who wait, hedge, and delay commitment spend all of MS4 trying to compensate.
Specialty‑Specific Nuances to Watch During MS3
Ortho
- Operative volume is high; you need to show you can function in a busy team.
- Programs care a lot about Step 2 and letters from known ortho faculty.
- A few good ortho research experiences matter more than 10 random posters.
ENT
- Smaller world. Reputations matter.
- Many departments expect you to have at least some ENT‑specific research.
- Your communication skills and fit with the team culture are scrutinized hard.
Plastics (Integrated)
- This is the top tier of competitiveness. Marginal numbers plus zero research is a non‑starter.
- Early mentor relationship is almost mandatory.
- You must be honest: if your metrics are modest, consider independent plastics later via general surgery or another pathway instead of trying to force an integrated slot.

How to Use the Rest of MS3 If You Are Already Behind
Maybe you are reading this in Month 9 of MS3. You did not honor surgery. You have no research yet. You are suddenly pretty sure you want ENT.
You are not dead. But you do not have room for denial.
At this point you should:
Run a brutally honest gap analysis with a mentor.
- Show them your grades, Step 1, practice Step 2, CV.
- Ask: “If I still aim for [specialty], what exactly would I need to do in the next 9–12 months to have a fighting chance?”
Concentrate your efforts.
- One specialty.
- 1–2 realistic aways.
- One focused research lane.
Decide on a clear backup and whether you would dual‑apply.
- Some people dual‑apply ENT + prelim surgery, or plastics + general surgery.
- Dual‑applying poorly (scattered story, mismatched letters) is worse than committing to one and owning the outcome.
Pulling It Together: Your MS3 Surgical Year Checklist
To make this concrete, here is what you should have accomplished by each major point.
| Time Point | Ortho/ENT/Plastics Readiness Markers |
|---|---|
| End of Month 2 | Identified mentors; primary and backup interests set |
| End of Surgery Block | Strong evals; 1–3 potential letter writers |
| Month 6–7 | Home sub-I month planned; away rotation target list |
| Month 7–9 | Declared primary specialty; research in progress |
Right now, do one concrete thing: open your calendar for the rest of MS3 and label the month when you will finish core surgery, the month you will do your home sub‑I, and the window you will submit away rotation applications. Then ask yourself: “Given where I am today, what has to happen before each of those dates for ortho, ENT, or plastics to still be realistically on the table?”





















