
The most dangerous place for an intern is not the bedside. It is the order entry screen at 2:13 a.m.
You will not fail your intern year because you do not know the dose of ceftriaxone. You will fail it because you waste 40 minutes rewriting the same admission orders, hunting for the right DVT prophylaxis, or fixing avoidable lab/consult mistakes that should have been solved with smart order sets and habits.
Let me break this down specifically.
The Core Reality: Interns Live (and Die) in Order Entry
Your schedule feels like: preround, round, write notes, enter orders, clean up orders, respond to pages about orders you already put in. The cognitive load is not the medicine; it is the workflow.
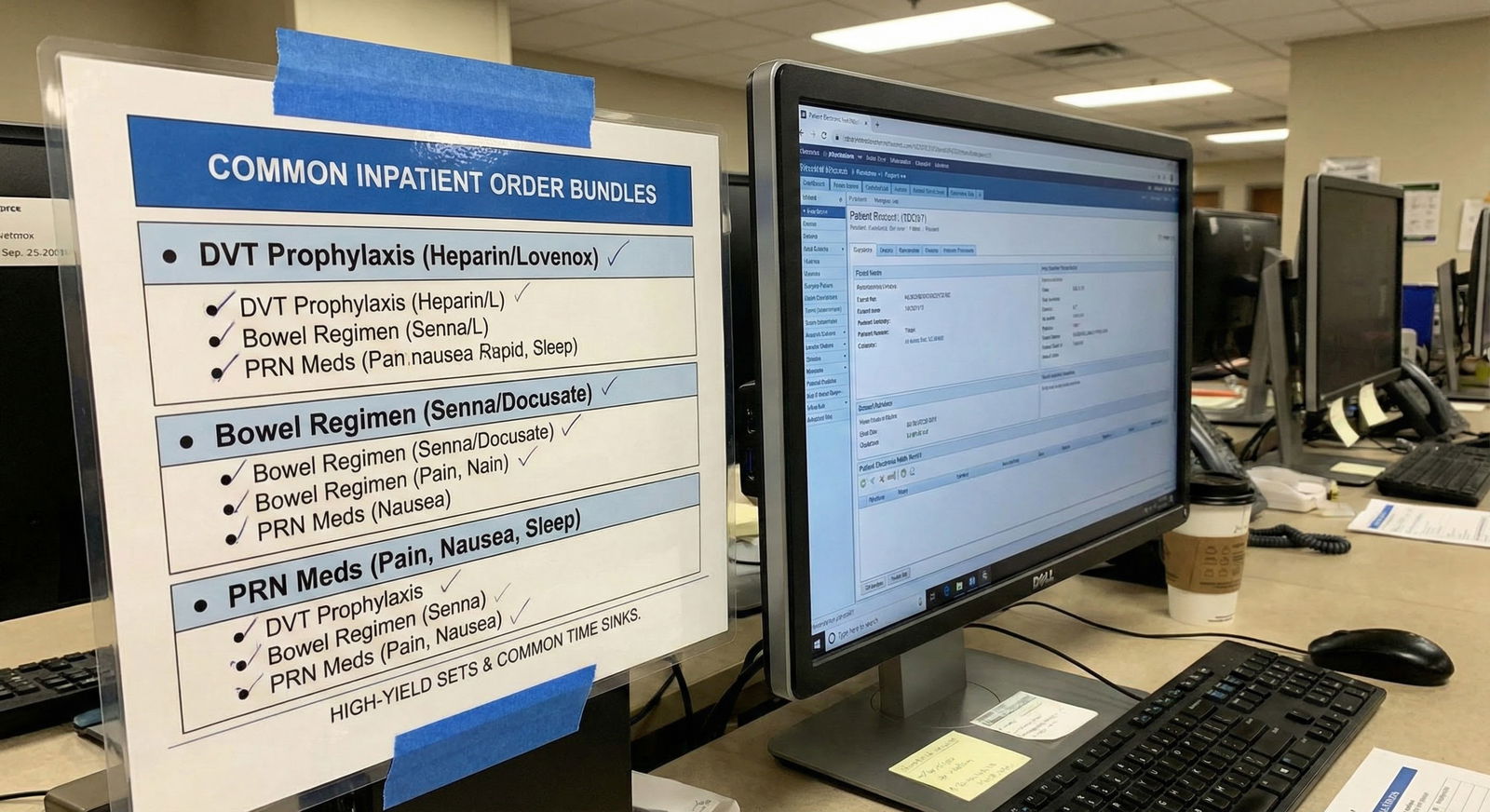
Two truths:
- There are a small number of high-yield order “bundles” you use over and over.
- There are predictable order entry time sinks that destroy your day if you do not systematize them.
You are not trying to be clever here. You are trying to be fast, safe, and boringly consistent.
High-Yield Admission Order Sets You Should Practically Memorize
Everyone’s EHR (Epic, Cerner, Meditech, Allscripts, whatever) has different names, but the patterns are universal. You want mental templates. So even when the EHR order set is trash, you know exactly what to add.
1. Generic Internal Medicine Admission Bundle
You will use this on half your admits.
Core pieces:
- Level of care and vitals
- Diet and activity
- Fluids and lines
- Labs and imaging
- DVT prophylaxis
- Bowel regimen
- Pain / nausea control
- Code status and communication
Think in this sequence when you open the admission screen.
Basic template (adapt as needed):
Level of care:
- Admit to: Medicine Team X, floor vs stepdown vs ICU
- Vitals: q4h or q8h; continuous pulse ox if respiratory issues
Diet / activity:
- Diet: Regular vs renal vs cardiac vs carb-controlled vs NPO (with “NPO except meds” if needed)
- Activity: Ambulate with assist vs bedrest with bathroom privileges
Fluids:
- Maintenance IV (if needed): e.g., Lactated Ringers 75–100 mL/hr vs “SLIV” only
- IV access: peripheral IV if not placed yet
Labs:
- Baseline: CBC, BMP, Mg, Phos
- Add: LFTs if any hepatic/biliary issue, coags if bleeding risk or anticoagulation coming, type & screen if bleeding/anemia
- Frequency: daily labs vs specific days; do not reflexively order "daily everything forever"
DVT prophylaxis:
- Enoxaparin 40 mg SC daily (or 30 mg BID / renal adjusted) vs heparin 5000 units SC TID
- Mechanical only if bleeding risk
Bowel regimen:
- Polyethylene glycol daily PRN or scheduled
- Senna at bedtime PRN
Symptom control:
- Pain: Tylenol PRN mild, opioid PRN moderate-severe with appropriate parameters
- Nausea: Ondansetron PRN
- Sleep: Trazodone or melatonin PRN if your hospital allows; be judicious
Code status / communication:
- Code status: Full vs DNR/DNI etc, with proper legal documentation
- Consults: case management / social work for high-risk discharges
If your EHR has a “Med Admission” or “Adult Admit” order set, great—use it but do not assume it has everything. Add your bowel regimen, DVT ppx, and PRNs proactively.
2. Pneumonia Admission Orders (CAP/HAP)
Pneumonia admissions are order-heavy but repetitive. You should have a pattern.
Core components:
Diagnostics:
- CXR (already done in ED? Ensure it is not pending.)
- Baseline labs: CBC with diff, BMP, Mg, Phos
- If moderate-severe: blood cultures x2, lactate
- Sputum culture if they are actually producing sputum
- Legionella and pneumococcal urinary antigen for severe CAP or ICU-level
Antibiotics (hospital-specific, but principles are similar):
- Non-ICU, no MRSA/Pseudomonas risk:
- IV ceftriaxone + azithromycin OR IV levofloxacin monotherapy (if QT risk etc)
- Healthcare-associated / HAP patterns:
- Add anti-pseudomonal (e.g., cefepime, piperacillin-tazobactam) ± MRSA coverage (vancomycin) based on risk factors
- Always:
- Enter indication (“CAP”, “HAP”) and intended duration (e.g., 5 days) so someone stops them on time
- Non-ICU, no MRSA/Pseudomonas risk:
Supportive orders:
- O2: goal saturation range (e.g., 88–92% in COPD, >92% in others)
- Nebs: albuterol/ipratropium PRN if wheezing
- Steroids: only if indicated (COPD/asthma overlap, septic shock, etc.), not automatic
Monitoring:
- Vitals q4h, pulse ox continuous if hypoxic
- Daily weights in heart failure or fluid-sensitive patients
The time sink here is antibiotic indecision. Decide the regimen once (with your senior/attending), memorize the standard doses, and use the same pattern unless there is a clear contraindication.
3. Heart Failure Exacerbation Orders
HF exacerbation admits are either smooth or a disaster depending on how clean your orders are.
Key pieces:
Diuresis:
- IV loop diuretic: furosemide IV (1–2x home PO dose if chronically on it) or equivalent bumetanide
- Specify: dosing interval and PRN extra dose instructions if responding poorly
- Daily weights and strict I/Os
Monitoring:
- Vitals q4h, pulse ox
- Daily BMP, Mg
- Telemetry if new arrhythmia, significant decompensation, or moderate-severe exacerbation
Fluid/salt:
- Diet: low sodium
- Fluid restriction (e.g., 1.5–2 L/day) if volume overloaded
Home meds:
- Hold vs continue:
- Often continue beta-blocker unless in shock or bradycardic
- Consider holding ACEi/ARB/ARNI if hypotensive or AKI
- Clarify with attending early, not at discharge
- Hold vs continue:
Imaging and labs:
- Repeat echo if last one outdated or if concern for new ischemic event or valvular issue
- BNP/NT-proBNP at baseline (useful but not something you keep checking daily without reason)
The expensive mistake: writing “daily labs” and never specifying when to stop. Put an explicit stop date or instruction in your brain: “reassess labs after 3 days.”
4. Diabetic Ketoacidosis / HHS Protocols
If your hospital has a DKA/HHS order set, use it religiously. This is not where you “freestyle.”
Typical components:
Insulin infusion protocol:
- Weight-based starting rate
- Titration parameters
- Protocol for dextrose addition when BG < 250–300 mg/dL
Fluid resuscitation:
- Initial bolus with isotonic fluid
- Ongoing fluid choices (NS vs half-NS) per protocol
Electrolyte monitoring:
- BMP, Mg, Phos every 2–4 hours initially
- Potassium replacement thresholds
“Transition to SQ insulin” section:
- Long-acting insulin overlap (start basal 1–2 hours before stopping drip)
- Meal-time insulin if eating
The time sink: piecemeal orders and constant “Please clarify DKA insulin” pages. One solid protocol order set solves 80% of that.
5. Alcohol Withdrawal / CIWA Protocol
If you are not using a protocol here, you are choosing chaos.
Typical set:
CIWA scale monitoring:
- Nursing orders for CIWA scoring interval (e.g., q1–4h)
- Clear thresholds for benzodiazepine dosing (e.g., lorazepam based on score)
Vitamin/electrolyte orders:
- Thiamine IV (before glucose if they are malnourished)
- Folic acid
- Magnesium repletion
PRNs:
- Antiemetic
- Antipsychotic PRN for severe agitation if protocolized and safe
Stopping point matters. Make sure there is a de-escalation plan once CIWA scores are low for 24 hours; otherwise they sit on CIWA and benzos forever.
High-Yield Daily “Maintenance” Order Sets
These are the background orders you will re-use on basically every inpatient.
1. DVT Prophylaxis: Decide Once, Default Hard
Nothing wastes more intern time than re-arguing basic prophylaxis decisions.
Your mental algorithm:
Normal renal function, average patient:
- Enoxaparin 40 mg SC daily.
Renal impairment (CrCl < 30):
- Enoxaparin 30 mg SC daily or switch to heparin 5000 units SC BID/TID (per institutional practice).
High bleeding risk:
- Mechanical only: SCDs; document the rationale.
If your EHR has “Adult VTE Prophylaxis” order set that forces a risk stratification, learn the paths during orientation. Do not click random boxes just to dismiss the alert.
2. Bowel Regimen: Stop Creating Constipated Opioid Zombies
Intern mistake #1 on surgical co-management or pain-heavy services: opioids without bowel prophylaxis.
Simple schema:
Start:
- Polyethylene glycol 17 g PO daily
- Senna 1–2 tabs PO at bedtime
If no BM x 48 hours:
- Add PRN bisacodyl suppository
- Consider scheduled dosing instead of PRN
Add a quick text macro in your brain: “opioid = bowel regimen.” That pairing should be reflexive.
3. IV Fluids: Be Explicit, Not Lazy
“NS at 125 mL/hr” for everyone is lazy medicine. And it backfires.
Better pattern:
Resuscitation vs maintenance vs none:
- Resuscitation: bolus orders (e.g., LR 500–1000 mL over 1 hr), with re-assessment note.
- Maintenance: weight-based (roughly 1–1.5 mL/kg/hr), adjust for heart failure/CKD.
- None: if they are eating and drinking and not hypotensive, “saline lock IV” is enough.
Add stop dates or conditions:
- “Continue until tolerating PO”
- Put a task for yourself: “Reassess fluids on rounds” and actually change the order.
Time sink you avoid: hours of diuresis later for fluid you mindlessly poured in.
Lab and Imaging: Where Intern Time Goes to Die
Order entry for labs and imaging is where the system punishes the unfocused. You want to think in bundles, frequency, and stop dates.
1. Labs: Daily Forever Is Not a Strategy
Create mental categories:
One-time labs:
- Admission workup: baseline CBC, BMP, Mg, Phos, LFTs, coags, TSH, etc. Order once, not “daily” unless you have a reason.
Short-term daily labs:
- Acute kidney injury
- Electrolyte derangements
- Intensive diuresis
- New anticoagulation (e.g., heparin drip, DOAC initiation in complex patients)
No-need daily labs:
- Stable chronic anemia and no active bleeding
- Stable, uncomplicated pneumonia on day 4
- Young, low-risk post-op day 3 with normal labs
If your EHR allows “duration: 3 days” on standing labs, use it. If not, make “labs to cancel” part of your daily SOAP note and actually adjust.
2. Imaging Orders: Clear Indication, Right Priority
Common places interns flounder:
CT without contrast vs with contrast vs CTA:
- Know your service’s common patterns. Example:
- Suspected PE: CTA chest with PE protocol.
- Abd pain, r/o appendicitis: CT abd/pelvis with contrast (unless Cr too high / allergy).
- Do not waste 15 minutes hunting through radiology options every time. Ask senior once, write it down.
- Know your service’s common patterns. Example:
Priority:
- “STAT” is not a magic wand. Overusing it just annoys radiology and slows down real emergencies.
- Use:
- STAT: acute neuro changes, suspected perforation, hemodynamic instability.
- ASAP: urgent but not critical.
- Routine: the rest.
Big time sink: incomplete or vague indications. Write a real question: “R/o PE in 65-year-old on OCPs with acute pleuritic chest pain and tachycardia” beats “SOB.”
Medication Orders: Where You Lose Sleep (and Pages)
Interns get buried in pages about meds: missing home meds, duplicate meds, unclear PRNs.

| Category | Value |
|---|---|
| Missing home med | 30 |
| Pain/nausea PRN | 25 |
| DVT ppx clarification | 15 |
| Lab frequency change | 20 |
| Diet/fluids | 10 |
1. Home Medication Reconciliation: Do It Once, Do It Right
Pharmacy often helps, but you are responsible for sanity-checking.
Approach:
Reconcile on admission:
- Bring in: essential chronic meds (beta-blockers, anticonvulsants, thyroid hormone, insulin).
- Temporarily hold: ACEi/ARB in hypotension/AKI, metformin in renal dysfunction/contrast, DOACs in high-bleeding-risk situations.
Avoid these common mistakes:
- Ordering both home insulin regimen and a separate sliding scale without thinking. Decide on a coherent insulin plan.
- Continuing home sedatives (e.g., high-dose benzos or zolpidem) plus adding hospital sleep meds “just in case.”
Document explicitly in your note why you held something. Saves you questions on rounds and later accusations of “forgot to restart.”
2. Pain and Nausea PRN: Build Standard, Safe Ladders
Stop reinventing this every time.
A typical medical floor ladder:
Mild pain:
- Acetaminophen 650–1000 mg PO q6h PRN (watch hepatic function, total daily dose)
Moderate pain:
- Oxycodone low dose PO q4–6h PRN
- Or hydromorphone PO/IV with clear parameters for use
Severe pain:
- IV opioid PRN with lockouts and reassessment
Nausea:
- Ondansetron 4 mg IV/PO q6–8h PRN
- Metoclopramide as second-line if protocol allows
What kills your time: vague PRNs like “hydromorphone 0.5–1 mg IV q2h PRN pain,” leading to constant nurse-physician clarifications. Tighten your ranges and frequencies.
Consults and “Order Dependencies”: Hidden Time Traps
A lot of your wasted time is not medicine. It is poorly chained orders.
1. Consults That Require Specific Orders First
Examples I have seen repeatedly:
- Nephrology:
- You consult for AKI, but have not ordered a renal ultrasound or urine electrolytes. They call you back… to tell you to order those.
- Cardiology:
- You ask for “chest pain, r/o ACS” with no EKG or serial troponins ordered.
Fix: build mini-checklists for common consults. For “AKI consult,” you reflexively order:
- UA
- Urine sodium/creatinine (if your institution uses them)
- Renal ultrasound (unless totally clear pre-renal source)
Write these on a cheat sheet. Use them.
2. Orders That Trigger Other Workflows (And Pages)
You order:
- Blood cultures but forget to specify source or STAT pick-up → micro or nursing calls.
- “Restraints” without required assessment frequency → nursing calls.
- “NPO” without indication or stop condition → SLP, dietitian, and nurses all call.
Solution: wherever your EHR pops up required fields or linked orders, do not speed-click through them. Those 10 seconds save you three pages.
Classic Time Sinks in Order Entry (And How To Kill Them)
This is the part nobody teaches. The stuff that makes you leave at 8 p.m. instead of 6 p.m.
| Time Sink | Fix Strategy |
|---|---|
| Rewriting admission orders | Create personal templates / macros |
| Vague PRN meds | Standardize ladders with clear dosing |
| Endless daily labs | Use time-limited orders and reassess |
| DVT ppx re-justification | Learn and follow local VTE algorithm |
| Incomplete consult orders | Build mini pre-consult checklists |
1. Rebuilding the Same Admission Over and Over
If your EHR allows:
SmartSets / order sets:
- Build your own personal “Medicine Admit – My Template” with your go-to:
- Diet
- DVT ppx
- Bowel regimen
- PRNs
- Standard labs
- Build your own personal “Medicine Admit – My Template” with your go-to:
SmartPhrases / Macros:
- At minimum, have:
.admitcore– baseline orders list you can modify..dischargecore– core discharge med + follow-up checklist.
- At minimum, have:
If your system is ancient and does not allow personalization, keep a physical or digital checklist. Crude, but faster than improvising.
2. Non-Stop Lab and Imaging Questions
A big portion of pages are “Do you still want daily X?” or “CT vs MRI?” at odd hours.
Pre-empt this:
In your daily progress note:
- Write a clear “Plan for labs/imaging”: “No further daily CBC; BMP tomorrow only for diuresis.”
- Nurses and night float will read this if they have any doubt.
In orders:
- Use comments on orders when possible: “Daily BMP x3 days while on IV diuresis; reassess afterward.”
Yes, this seems small. It saves you at 3 a.m.
3. Diet and Swallow Orders Chaos
Swallow evals, aspiration risk, and NPO decisions cause a ton of friction.

| Step | Description |
|---|---|
| Step 1 | Admit patient |
| Step 2 | Regular diet or restriction |
| Step 3 | Order SLP eval |
| Step 4 | SLP recommended diet |
| Step 5 | Keep NPO, consider feeding tube |
| Step 6 | Aspiration risk? |
| Step 7 | Safe swallow? |
Key strategies:
- If aspiration risk is suspected:
- Do not just write NPO and disappear. Enter SLP consult AND specify “NPO pending SLP.”
- After SLP:
- Update diet orders immediately to what they recommended.
- Cancel “NPO” if obsolete, so kitchen and nursing stop calling.
One of the most avoidable yet common pagers: “Diet order unclear after SLP note.”
4. Cross-Cover Orders That Haunt You
Night float interns lose the most time dealing with:
- Non-urgent cross-cover pages demanding immediate order changes for things that should have been settled daytime.
- Example: “Patient still in pain, no PRN beyond Tylenol,” at midnight.
- Example: “No sleep meds ordered for chronic insomnia patient who has been in the hospital 3 days.”
You cannot fix everything, but you can reduce this by:
- Adding PRNs thought-fully at admission.
- Anticipating:
- Night pain
- Nausea with new antibiotics
- Insomnia in high-risk patients (within reason)
Ask yourself before you sign out: “If I were night float, what would I hate about this patient’s orders?” Then fix those.
Using Your EHR Like a Competent Human, Not a Victim
The EHR is clunky, but it is also programmable. Learn its weapons.

| Category | Value |
|---|---|
| Week 1 | 0 |
| Week 2 | 15 |
| Week 3 | 25 |
| Week 4 | 30 |
1. Favorite Lists and Quick Orders
In Epic, Cerner, etc., you can favorite:
- Common labs:
- “CBC,” “BMP,” “Mg,” “Phos,” “Type & Screen,” “INR.”
- Common meds:
- Enoxaparin ppx doses
- Bowel regimen components
- Opioid + Tylenol + antiemetic bundle you use repeatedly
Set these up early. If you are still hunting for “CBC” in a giant list by month 3, you are just punishing yourself.
2. Order Panels and Personal Sets
If allowed, create:
- “Chest Pain Floor Admit” panel:
- Serial troponins
- EKG
- Telemetry
- Basic labs
- DVT ppx
- “COPD Exacerbation Admit” panel:
- Steroid regimen
- Antibiotic standard choice
- Nebs q4h + PRN
- O2 orders with target sat
First time takes 5–10 minutes. You will use them hundreds of times.
3. SmartPhrases that Tie Orders to Notes
Your note and orders should reflect each other. Use SmartPhrases that remind you about orders:
- Example:
.copdplantext:- “COPD exacerbation: steroids x5 days, antibiotics x5 days, scheduled + PRN nebs, O2 goal 88–92%, DVT ppx, bowel regimen.”
- As you type this, you naturally remember to place or correct those orders.
A good note template doubles as an order checklist.
Night Float and Cross-Cover: Special Considerations
Different game at night.

1. Cross-Cover Order Philosophy
You are not there to reinvent day team plans at 2 a.m.
General rules:
For non-urgent issues:
- Do the least disruptive, safest thing that bridges to morning.
- Example: one-time dose of sleep med for distressed chronic insomniac + note “please reassess chronic insomnia meds in AM.”
For potential safety issues:
- Check the chart quickly before ordering:
- Hypotension and “need more pain meds?” look at vitals, last doses.
- Confusion and “need sleep aid?” screen for delirium first.
- Check the chart quickly before ordering:
2. Rapid Responses and STAT Orders
These are where your order entry skills either shine or embarrass you.
Minimum bundles you should know cold (often in an RRT order set):
- For acute hypotension:
- STAT vitals
- STAT EKG
- STAT lactate
- STAT CBC/BMP
- Blood cultures if sepsis suspected
- Fluid bolus orders
- For acute respiratory distress:
- ABG or VBG
- Portable CXR
- O2 escalation orders (nasal cannula to HFNC/BiPAP per policy)
- Nebs if wheezing
Practice mentally: if you had to order these in 30 seconds, could you? If not, shadow a senior or ask someone to walk you through the hospital’s RRT order sets.
Putting It All Together: A Realistic Admission Example
Let me walk you through a classic scenario and how a competent intern handles order entry.
Case: 68-year-old with CAP, CHF, Diabetes
ED is boarding. You are told: “Admit to medicine.”
Your order sequence:
Level of care:
- Admit to medicine floor, vitals q4h, continuous pulse ox (mild hypoxia).
Diet and activity:
- Cardiac/carbohydrate-controlled diet.
- Ambulate with assist.
Fluids:
- No continuous fluids; they got 2L in ED and have HF. “SLIV only.”
Labs:
- One-time: CBC, BMP, Mg, Phos, LFTs.
- Daily BMP x3 days while on IV diuretics (if you diurese for CHF overlap).
Imaging:
- Confirm CXR completed; if not, order portable CXR.
Antibiotics:
- Ceftriaxone + azithromycin order set, indication “CAP,” planned duration 5 days, renal dosing verified.
DVT prophylaxis:
- Enoxaparin 40 mg SC daily.
Diabetes management:
- Basal insulin: continue home glargine dose with correctional sliding scale.
- Hold metformin if AKI or recent contrast.
Bowel regimen:
- Polyethylene glycol daily, senna at bedtime PRN.
PRN meds:
- Tylenol for mild pain/fever.
- Oxycodone low dose PRN moderate-severe pain.
- Ondansetron PRN nausea.
- Code status:
- Full code for now (until discussion), document “To be discussed with patient/family on morning rounds” if not clarified.
- Consults:
- None right now; case management consult next day if complex social situation.
That is 5–7 minutes with decent EHR skills. Not half an hour of flailing.

FAQs
1. How do I avoid missing key admission orders when I am rushed?
Create a simple, 1-page checklist you keep at your workstation or in your pocket. Include: level of care, vitals, diet, DVT ppx, bowel regimen, PRNs, labs, and code status. Use it for every admission until it is automatic. If your EHR allows personal order sets, build a “General Admit” set and use that as your default starting point.
2. What is the most common medication-related order mistake interns make?
In my experience: forgetting DVT prophylaxis or bowel regimens when starting opioids. Close second: sloppy pain PRNs with huge dosing ranges and unclear frequency. Both generate extra pages and patient harm risk. Fix this with a simple rule: every opioid gets a bowel regimen; every floor admit gets a VTE prophylaxis decision documented.
3. How much should I rely on pre-built hospital order sets?
Use them heavily but not blindly. They are great for structure, terrible when applied uncritically. Open the order set, remove what does not apply (e.g., unnecessary daily LFTs), and add the things they weirdly omit (like bowel regimens or targeted PRNs). Think of order sets as a scaffold, not a finished building.
4. What can I do during orientation month to make order entry easier later?
Spend one dedicated hour creating favorites: labs, common meds, your go-to prophylaxis, PRN meds, admission bundles. Shadow a senior resident entering real orders and ask them to narrate their clicks. Build at least one personal order panel (e.g., “Medicine Admit”) and test it on a low-stakes patient. That one hour saves you tens of hours over the year.
5. How do I manage order entry safely when I am completely exhausted on nights?
Fall back on protocols and checklists. Use your hospital’s standardized RRT, DKA, sepsis, and alcohol withdrawal order sets. When your brain is mush, avoid freestyle complex insulin regimens or polypharmacy. If something feels risky, call your senior. Your job at 3 a.m. is to keep patients safe and alive, not to optimize every chronic condition.
6. How do I get faster without becoming sloppy?
Speed comes from patterns, not from rushing. Build a small set of high-yield templates for: general admits, pneumonia, CHF, COPD, DKA, ETOH withdrawal. Learn your EHR shortcuts (favorites, order panels, SmartPhrases). And after every call or night, pick one painful order-entry situation and ask: “How could I have systematized this?” Fix that one thing. Incremental improvements compound fast.
Key points: order entry is where interns truly live, and a small number of standardized bundles cover most of what you do. Build personal systems—templates, checklists, and smart use of EHR tools—to kill repetitive time sinks. The goal is simple: be fast, be safe, and stop letting the order screen control your life.



















